Findings In Lung Ultrasound That Predict A Poor Prognosis In Patients With Covid-19
PURPOSE OR OBJETIVE:
To establish the findings of lung ultrasound (LUS) and the final outcome in patients with a diagnosis of COVID-19.
Methods: This is a descriptive, prospective, longitudinal study. We studied all patients admitted to the health center who were diagnosed with COVID-19 and who underwent LUS. These 13 patients were evaluated by lung ultrasound and the US findings were associated with the final evolution of the patient.
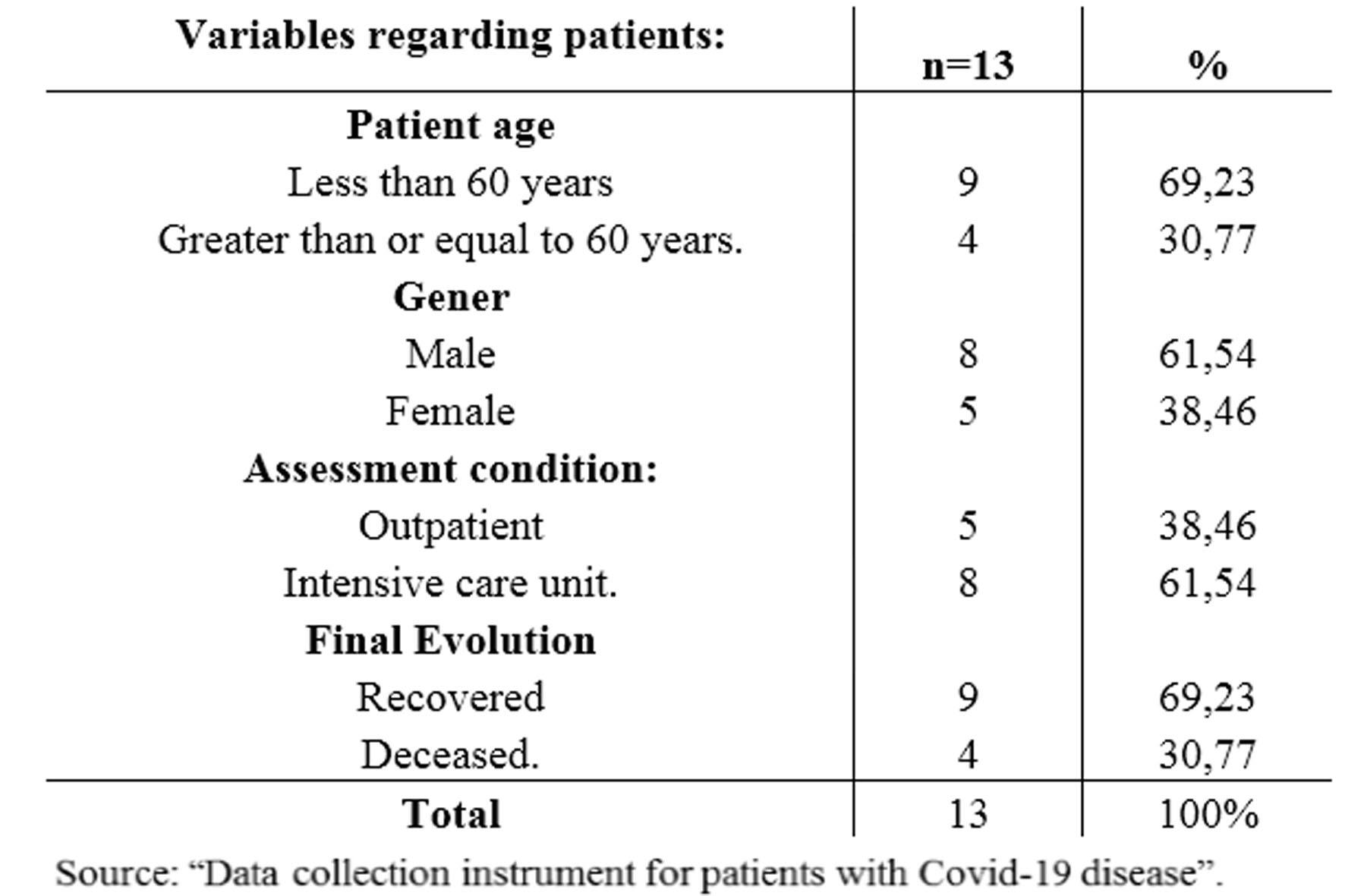
Results: 13 patients were evaluated, 8 (61.57%) men and 5 (38.46%) women, between 30 and 86 years old, with 1 to 4 follow up ultrasounds. 9 recovered and 4 died.
A statistically significant relationship was demonstrated between: death as the final outcome and the presence of 11 or 12 affected areas of the 12 evaluated by LUS, regardless of the pathological pattern they presented (p <0.01). A statistically significant relationship was demonstrated between death as the final outcome of the patient and the presence of subpleural consolidations in at least 6 of the 12 areas evaluated by LUS during follow up (p <0.05).
Conclusion: The presence of 11 or 12 areas affected by any pathological pattern on LUS and the presence of 6 or more areas with subpleural consolidations are ultrasound factors of poor prognosis in patients with COVID-19 disease. (p <0.01) and (p <0.05) respectively.
Keywords:
COVID-19, Lung, Ultrasound, severe acute respiratory syndrome coronavirus 2.
Key points:
Pulmonary ultrasound helps predict poor prognosis in COVID-19
Abbreviations and acronyms:
WHO: World Health Organization.
LUS: Lung ultrasound.
LUSS: Lung ultrasound score.
CT: Computed tomography.
INTRODUCTION
There have been millions of cases in the world of the novel coronavirus disease (COVID- 19). On October 25th 2020, the WHO reported more than two million new cases of COVID-19. In the seven days prior to this, there were 42 million cases and 1.1 million deaths from COVID-19 in the world. (1) It was declared a pandemic by the World Health Organization (WHO) on March 11, 2020. (2) Because COVID-19 has led to a pandemic, a lot of information is necessary to achieve its control and the recovery of a greater number of patients. COVID-19 can cause acute respiratory distress syndrome (ARDS), increasing admissions to intensive care units, as well as causing death. Among the main imaging methods for evaluating the lungs, we have simple or high-resolution tomography and chest radiographs. The predominance of peripheral pulmonary disease has been described, therefore the use of lung ultrasound (LUS) was implemented as a study method in patients with COVID-19. (3)
Considering the saturation of tomography services during the pandemic, even with availability of such equipment in health centers, these areas could saturate their capacity. In many countries, due to economic limitations, lack of accessibility or poor maintenance, as well as the absence of adequately trained personnel, there are places without resources such as computed tomography (CT) or X-ray equipment and this favors the use of the ultrasound (US) and begins to take on greater importance as an assessment instrument for patients with COVID-19.
Multiple aspects make us consider US as a very useful tool, essential in evaluating the evolution of patients with COVID-19. International organizations and expert meetings have highlighted the usefulness of LUS for the diagnosis, management and monitoring of pneumonia due to COVID-19. There is evidence of the comparable capacity of LUS with chest radiographs or CT for the evaluation and follow-up of predominantly peripheral pleural or parenchymal pathology. (4,5,6,7)
The use of US in patients with COVID-19 has great advantages; Low-cost equipment, greater availability, it does not emit ionizing radiation and allows the assessment of patients in real time. Ultrasound has a very important role in intensive care and it allows clinicians to monitor patients, assessing their evolution through imaging and establishing the most appropriate therapy early in patients with COVID-19.(2,7) In this respect, the lung ultrasound score (LUSS) can be used to assess the loss of lung aeration and quantitatively monitor its evolution in days. (8)
Based on this information, the following question arises: ¿How are the LUS findings related to outcomes in patients with COVID-19 who were assessed by the Ultrasound Service of the “El Paso” Medical Teaching Center, from August to October 2020?
MAIN OBJECTIVE
To analyze the findings of LUS and the outcomes of patients with a diagnosis of COVID- 19 who were assessed by the Ultrasound Service of the “El Paso” Medical Teaching Center, from August to October 2020.
SPECIFIC OBJECTIVES
Characterize the distribution by age groups and gender of patients diagnosed with COVID-19.
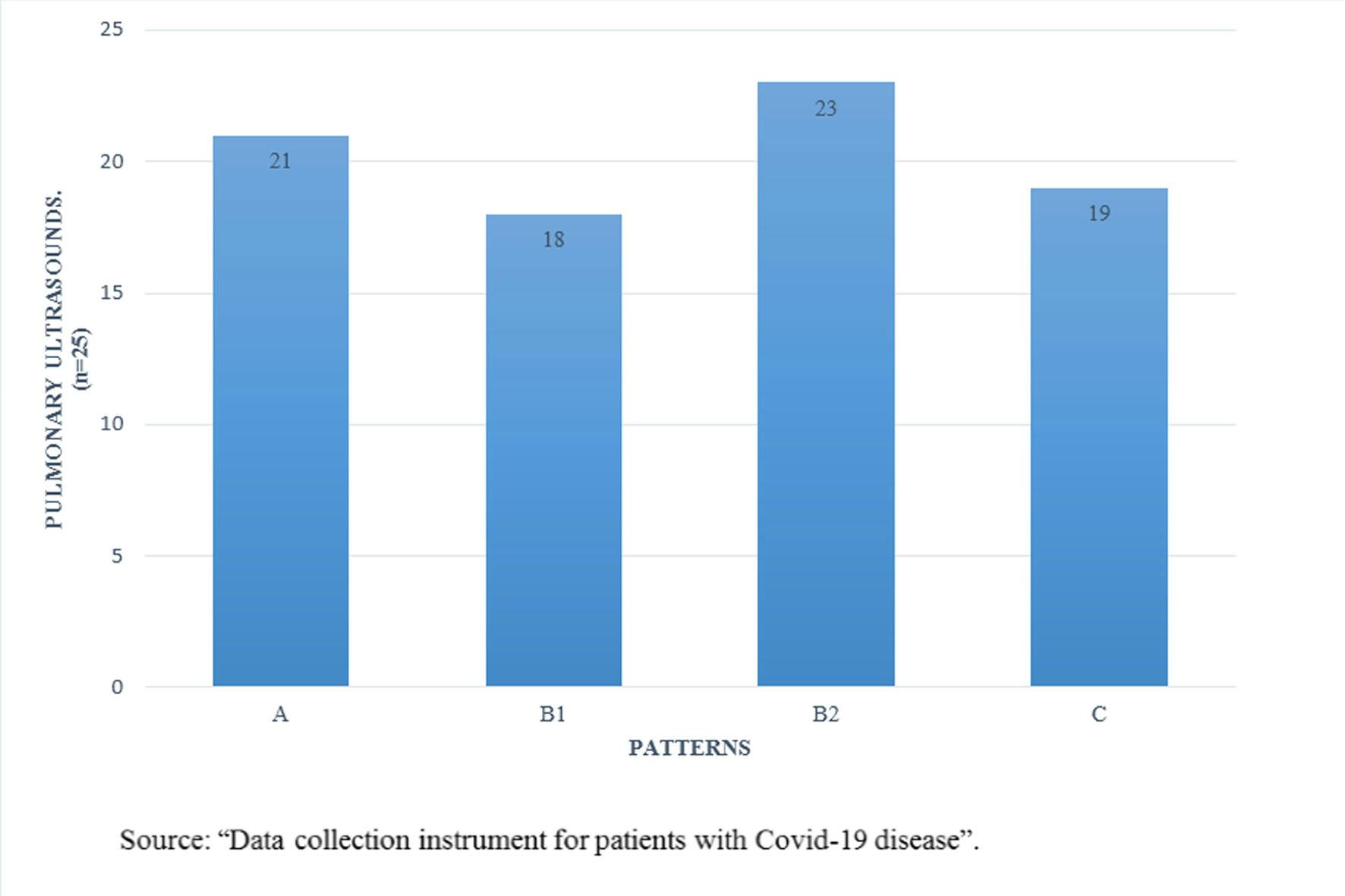
Identify the most frequent pulmonary ultrasound patterns in patients diagnosed with COVID-19.
Identify lung ultrasound findings associated with poor prognosis in patients diagnosed with COVID-19.
Relate the pulmonary ultrasound score with the final evolution of patients diagnosed with COVID-19.
METHOD
Type of study:
Prospective, descriptive and longitudinal study.
Population and sample:
The population was made up of all the patients with a diagnosis of COVID-19, who attended the Ultrasound Service of the “El Paso” Medical Teaching Center, from August to October 2020, from whom LUS was requested. The sample is intentional, not probabilistic, limited to the number of cases presented in the study period, corresponding to 13 patients.
Inclusion Criteria:
Patients with a diagnosis of COVID-19 who had lung ultrasounds requested.
Exclusion Criteria:
Patients who did not consent to being included in the study. Patients without a diagnosis of COVID-19 for whom lung ultrasounds were requested.
MATERIALS AND METHODS:
All patients with a diagnosis of COVID-19 who attended the Ultrasound Service of the “El Paso” Medical Teaching Center with a request for a LUS were included in the sample. Patients who did not consent to participate in the study were excluded. Thisteen patients were evaluated, 8 admitted to the Isolation area for COVID-19, Intensive Therapy Unit, and 5 were evaluated as outpatients; successive US controls were carried out; between 1 and 4 evaluations. The in-hospital stay varied between 1 and 19 days and LUS was performed according to the requirements of the medical personnel in charge. Chest CT was performed, with a "Siemens" brand equipment, to support the ultrasound findings, when the staff considered it necessary, always based on the principles that establish the minimum dose necessary of radiation for diagnosis. These data were recorded in the LUS reports of patients with a diagnosis of COVID-19, stored and organized, to later be compiled in the “Data collection instrument for patients with COVID-19”. This instrument recorded patient identification, age, gender, LUSS, predominant ultrasonographic pattern, time of hospital stay, dates of admission and discharge, as well as the final outcome of the patient (recovery or death).
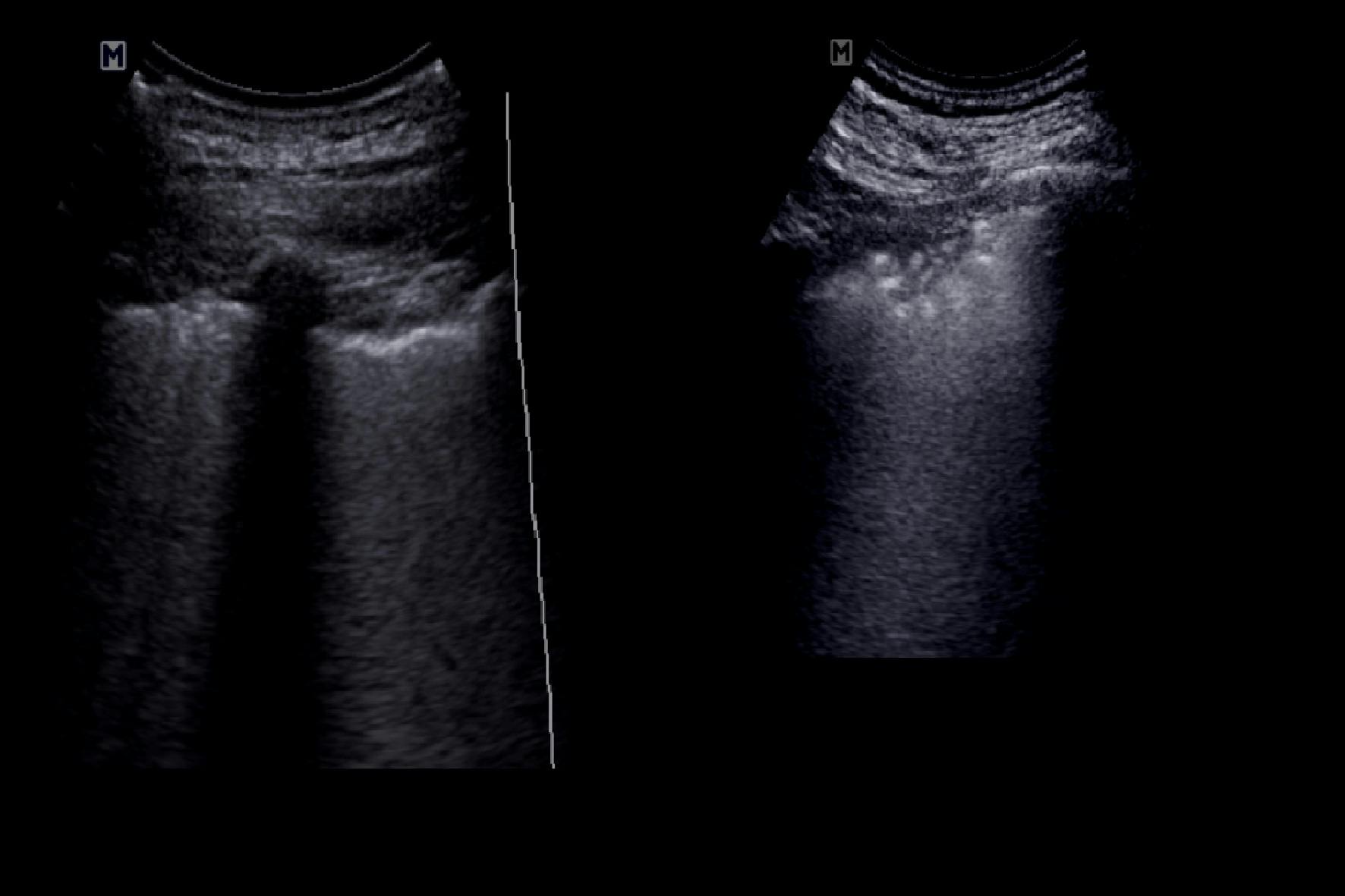
The ultrasounds were performed using a brand: "Medison", model: "Acuvixx", with volumetric and linear multifrequential transducers, at the discretion of the radiologist. The evaluation was performed using LUS, as established, dividing each hemithorax into 6 regions: upper anterior, lower anterior, upper lateral, lower lateral, upper posterior and lower posterior. In each region, the presence of "A" lines was assessed, in relation to pattern "A", corresponding to adequate pulmonary aeration; normal lung. The presence of 3 or more separate "B" lines, in relation to the "B1" pattern, suggestive of moderate loss of pulmonary aeration; mild interstitial syndrome. The presence of 3 or more confluent or coalescing “B” lines, suggestive of a “B2” pattern, corresponding to severe loss of pulmonary aeration; moderate - severe interstitial syndrome.

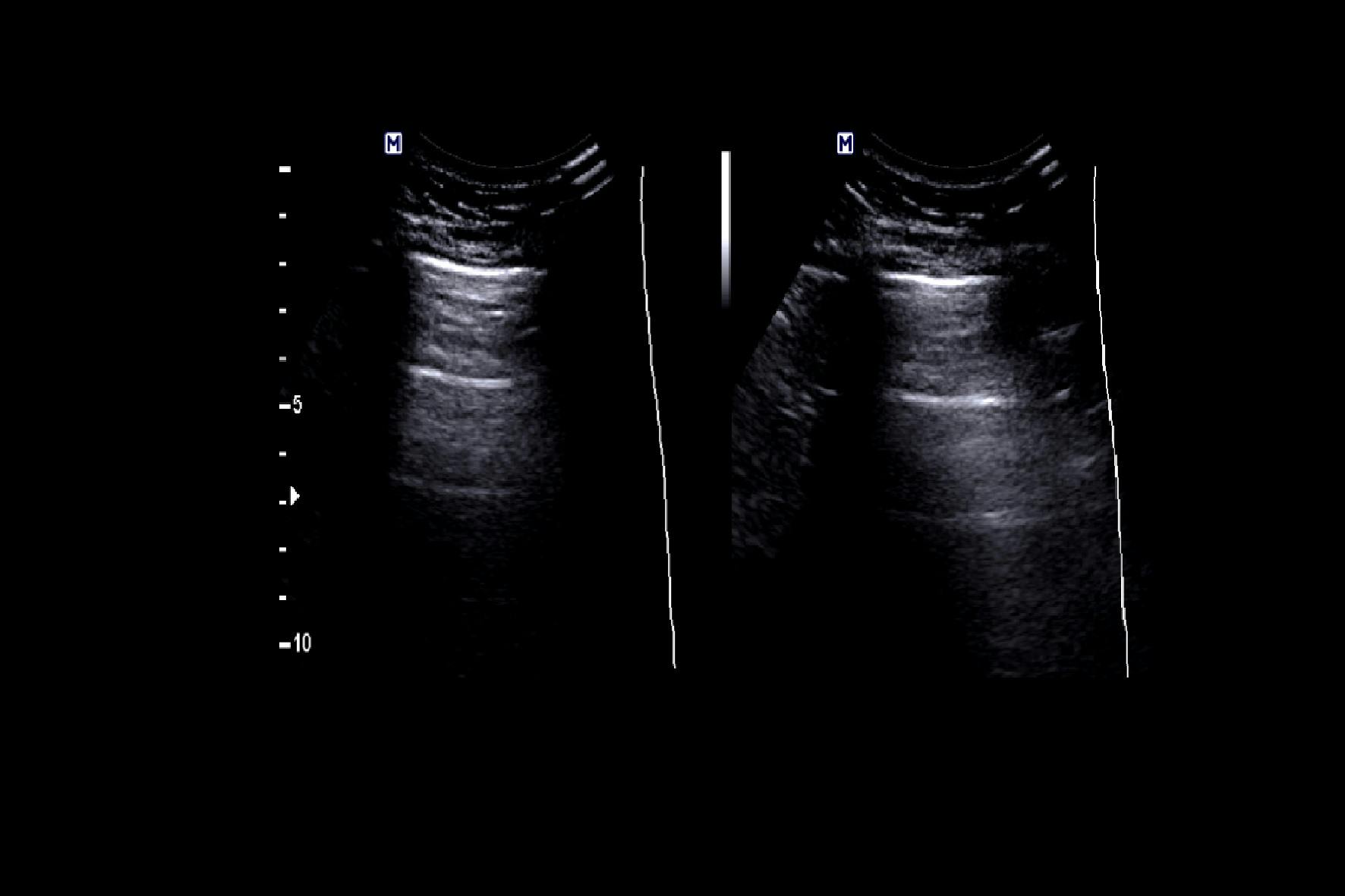

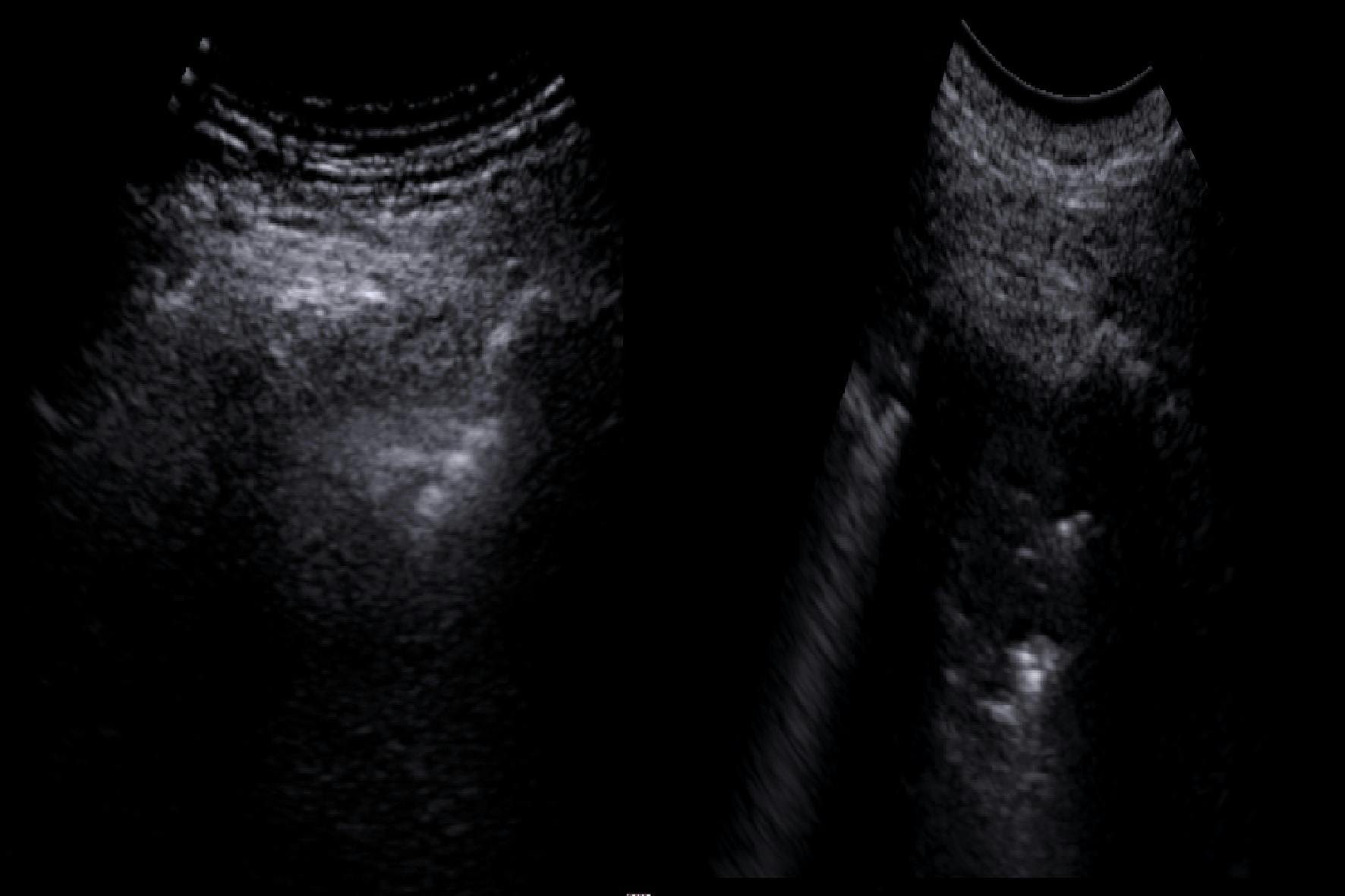
The visualization of a subpleural air bronchosonogram in relation to subpleural consolidations or hypoechoic areas in the lung with an air bronchosonogram sign, suggestive of consolidation, in relation to a “C” pattern (occupation of the alveoli by liquid content; alveolar syndrome, which conditions critical loss of lung aeration).
We assigned a value to each region corresponding to the highest pattern found. These patterns had the values of 0, 1, 2 and 3, respectively. The LUSS was calculated, adding the value corresponding to each region, varying from 0 to 36, with 36 being the value that indicates greater severity from the ultrasonographic point of view. (8, 9, 10) The information obtained was compiled in tables and graphs, all the variables considered pertinent were related, using the “Excel” Software from “Microsoft Office 2013”, and the Software “SPSS Statistics 22 from IBM” for the analysis of the statistical data. We then composed the results, discussion and conclusions.
MATERIALS:
Ultrasound equipment brand: "Medison", model: Accuvix, with volumetric and linear transducer, as well as computers.
Variables: Qualitative, dichotomous variables were established, as follows:
Patient variables:
Patient age: Less than 60 years / greater than or equal to 60 years.
Patient gender: Male / Female.
Final outcome of the patient: Recovered / Deceased.
Assessment condition: Outpatient / Intensive care unit.
Ultrasound variables:
LUSS: Less than or equal to 18 points / greater than 18 points.
Individual ultrasonographic pattern most frequently found: Pattern “A”; Pattern “B1”, Pattern “B2”; and Pattern “C”, with the indicator for each of these corresponding to: present / absent, based on the presence or absence of the aforementioned characteristics of each pattern, in each of the ultrasounds performed.
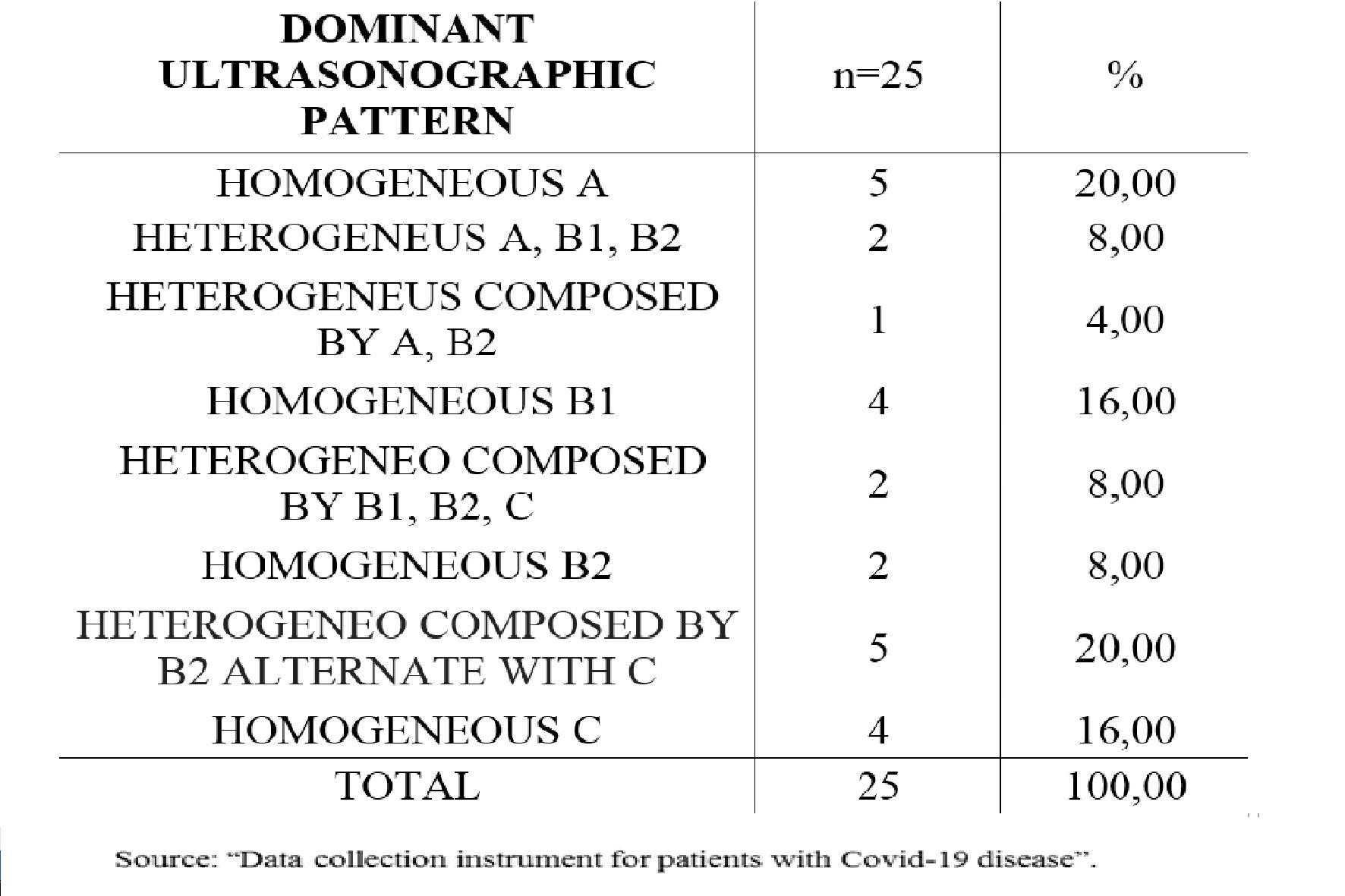
Predominant pattern according to its association: Homogeneous pattern "A"; Homogeneous "B1" pattern; Homogeneous "B2" pattern; Homogeneous pattern "C"; Heterogeneous pattern A, B1, B2; Heterogeneous pattern A, B2; Heterogeneous pattern B1, B2, C; Heterogeneous pattern B2, C, with the indicator in each of these corresponding to present / absent, referring to the presence or absence of each of these pattern associations, as the predominant pattern in each ultrasound performed.
Condition of 11 or 12 affected areas in the LUS of 12 areas: present / absent, according to the presence or absence of 11 or 12 areas in the ultrasound of 12 areas, with evidence of pathological images, regardless of the pathological pattern they present.
Condition of 6 - 12 affected areas with the presence of subpleural consolidations in the LUS of 12 areas: present / absent, according to the presence or absence of 6 or more areas with the ultrasonographic characteristics described above.
Statistical analysis:
The data were compiled in tables and graphs using the “Microsoft Excel” software. The "IBM SPSS Statistics 22" Software was used, by means of which the data was grouped in cross tables and associated as dichotomous variables. Fischer's exact test was used to assess statistical significance, considering those associations with statistically significant p less than 0.05, determining at least a 95% confidence interval.
RESULTS:
13 patients were evaluated, 8 (61.57%) male and 5 (38.46%) female. The age range was between 30 to 86 years with an average age of 63 years. In-hospital stay: 1 - 19 days, with 1 to 4 US follow ups. Eight (61.53%) patients were admitted to the Isolation area for COVID-19, Intensive Therapy Unit, and 5 (38.46%) were managed as outpatients. 9 (69.23%) patients recovered and 4 (30.77%) died.
The ultrasound pattern most frequently found individually, was pattern “B2”, corresponding to loss of severe pulmonary aeration. This pattern was visualized in 23 (92%) of the 25 ultrasounds performed during the controls.
The predominant pathological ultrasound pattern observed in most of the ultrasound studies was the heterogeneous pattern, given by areas of “B2” pattern, with subpleural consolidations, which was the predominant pattern in 5 (20%) of the 25 studies of ultrasound performed during successive evaluations of patients. Pattern “A” was found in the same proportion that Pattern “B2”, being the predominant pattern in 5 (20%) of the 25 ultrasounds performed in the patients evaluated during their follow up, due to the evaluations made at the onset of symptoms in a certain group of patients.
Four patients who presented during their evolution; 11 or more affected regions in the LUS from 12 regions, died, while only one of the recovered presented this condition. The LUSS itself was not relevant, nor was the type of pathological ultrasound pattern they presented. A statistically significant relationship was demonstrated between the presence of 11 or more affected areas of the 12 evaluated by ultrasound, during the controls, regardless of the pathological pattern they presented, during the controls with death as the final evolution. (p <0.01), with 99% confidence.
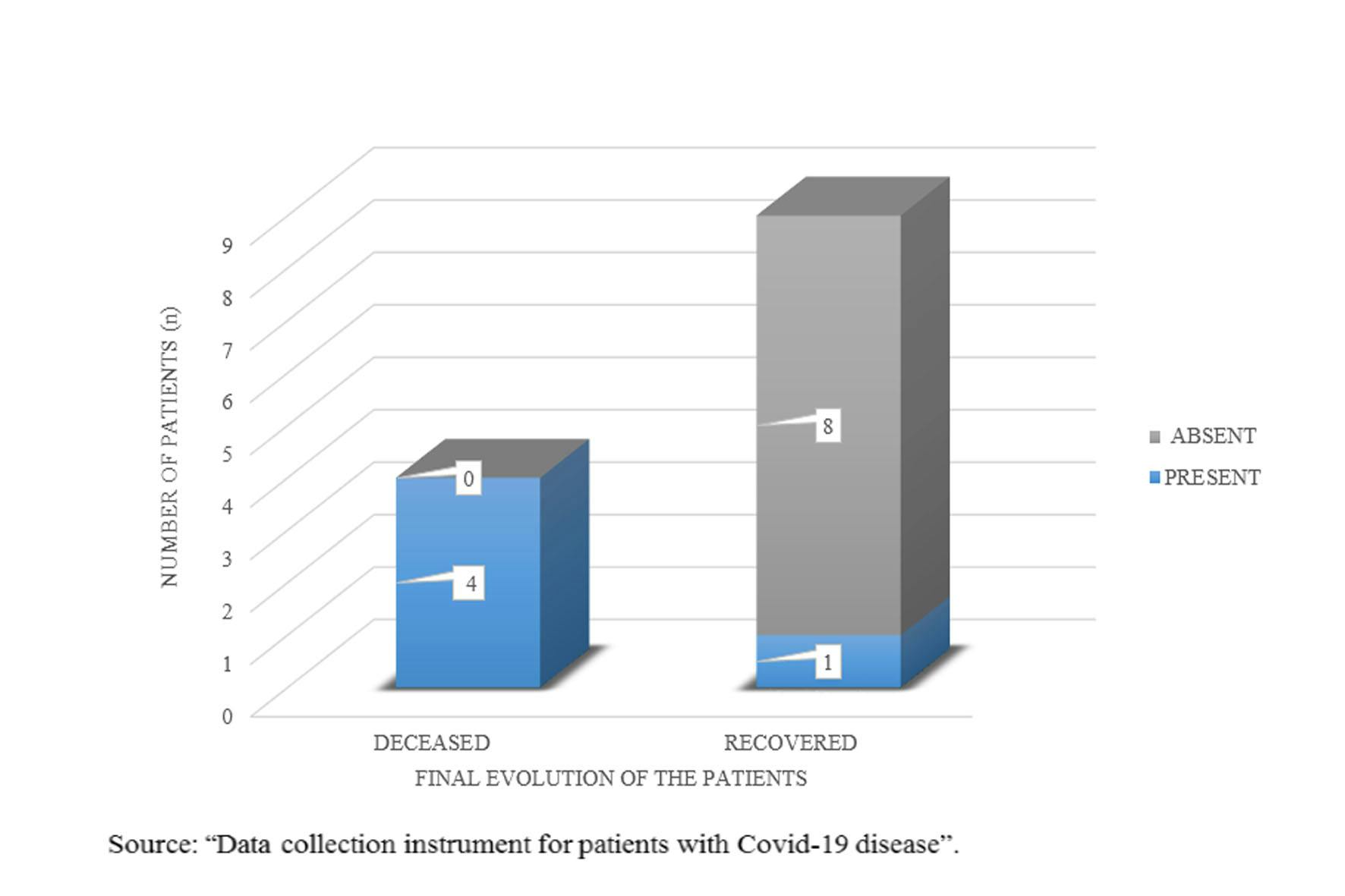
Of the 4 deceased patients, 3 (75%) had more than 6 areas with subpleural consolidations in the LUS. Of the 9 patients who recovered, none had 6 or more areas with subpleural consolidations in the LUS.
A statistically significant relationship was demonstrated between death as a final outcome and the presence of subpleural consolidations in at least 6 of the 12 regions evaluated by LUS during follow up (p <0.05), with 95% confidence.
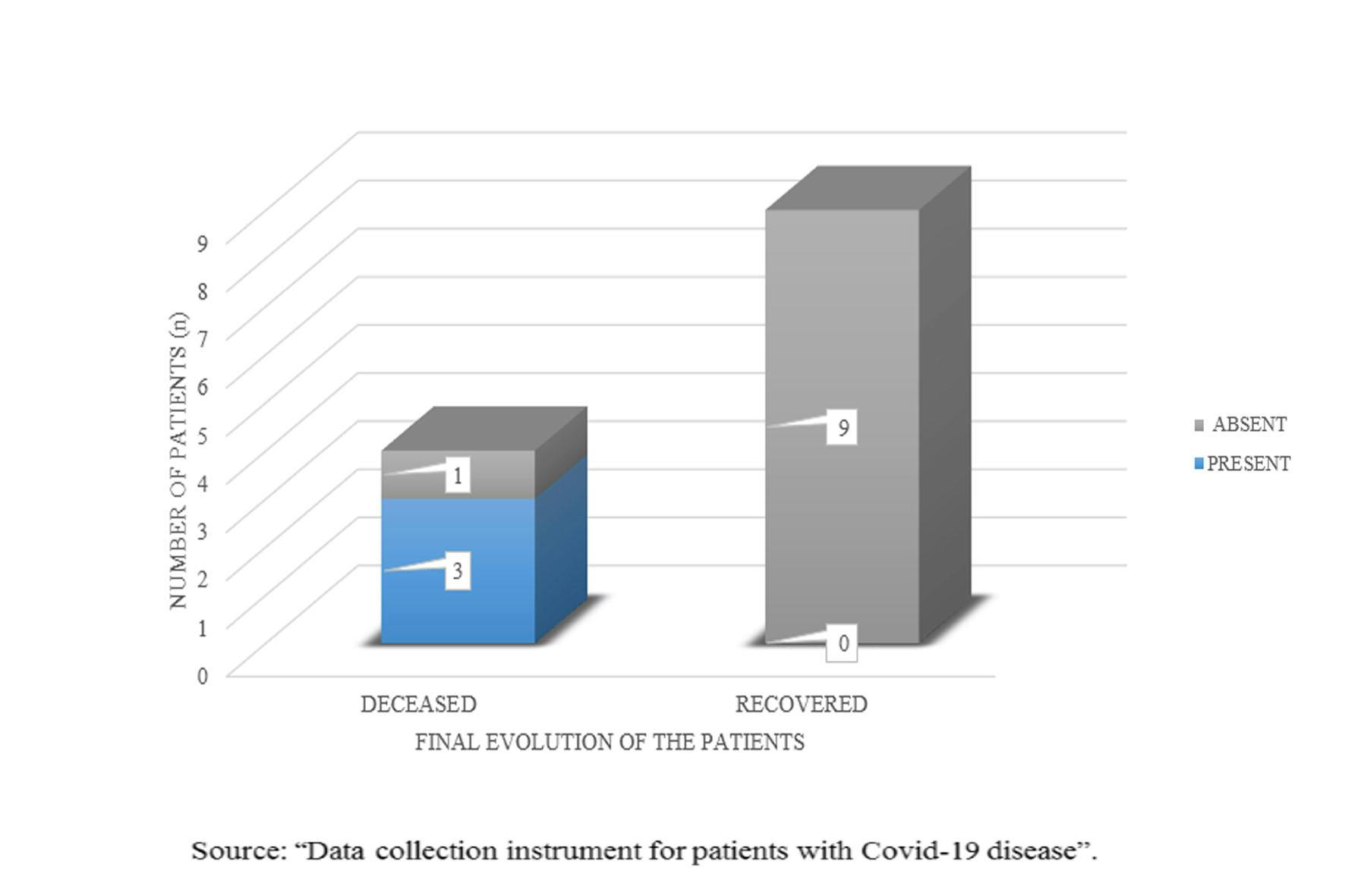
Therefore, it was established that the presence of 11 or 12 affected regions in the LUS during follow up, as well as the presence of 6 or more regions with subpleural consolidations, constitute ultrasound findings of poor prognosis for COVID-19.
No association with death was demonstrated in patients with a LUSS greater than 18 pointsat any time during the follow-up, in the evaluation of 12 spaces, (value of p = 0.9> 0.05).
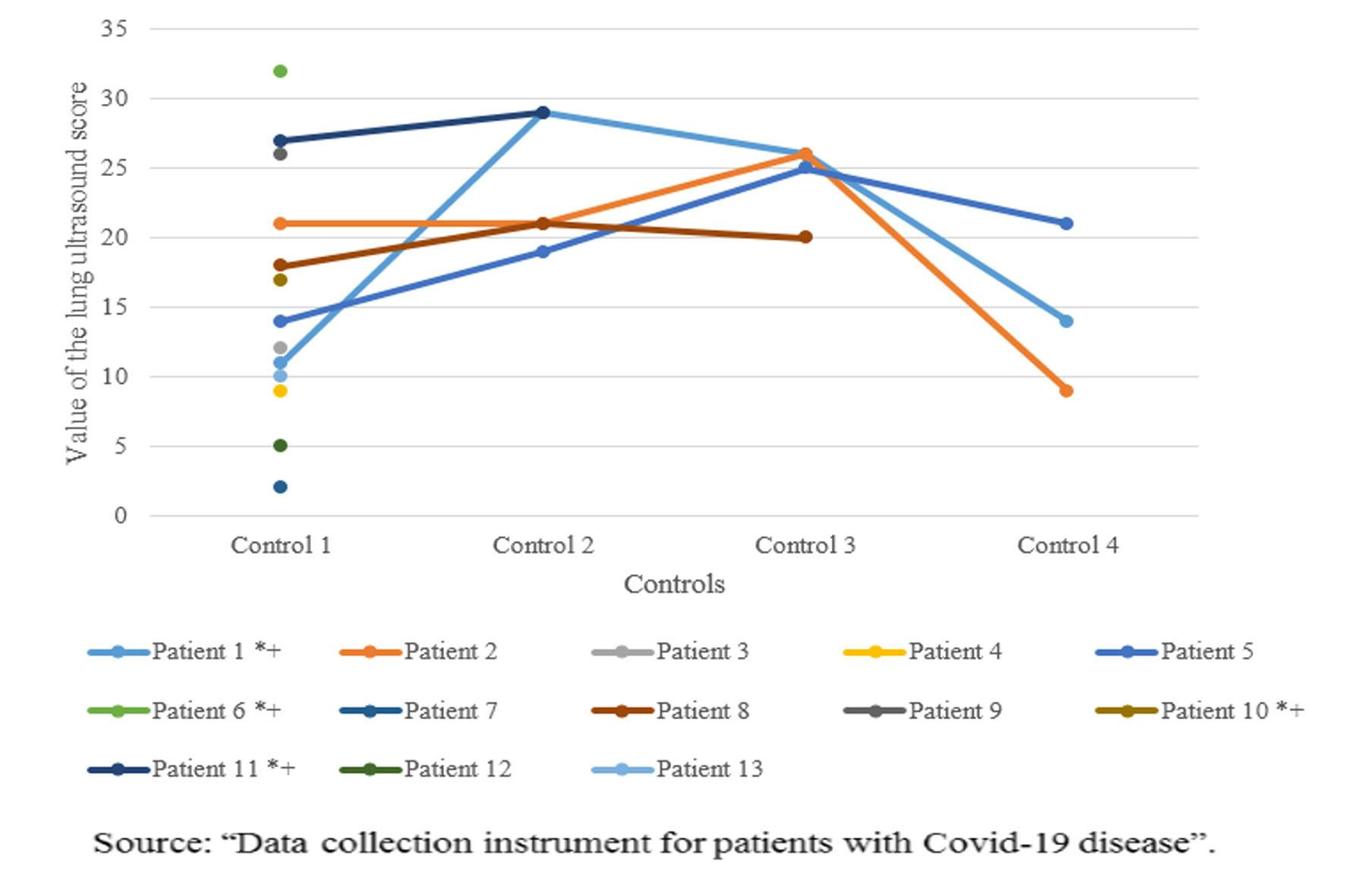
Death was not associated with gender (p=0.490> 0.05), with age older than 60 years (p=0.490> 0.05), or with the predominant pathological ultrasound patterns. The ultrasound pattern with the greatest statistical relevance (not yet significant) was the heterogeneous pattern constituted by "B2" alternated with "C" (p=0.07>0.05).
DISCUSSION:
The percentage of patients who died from COVID-19 was high: 30.7%, compared to the study by Ramos C et al (2) in which there were 9.1% of deaths.
The B2 ultrasonographic pattern (corresponding to severe loss of pulmonary aeration), was the most frequently visualized individual pattern in patients with COVID-19, coinciding with the study by Ramos C et al(2), in which the ultrasound sign most frequently found in patients with COVID-19 was the presence of B lines and it was visualized in 75% of the cases evaluated. To a lesser extent, the other typical patterns were observed, such as the “B1” pattern (corresponding to moderate loss of lung aeration) and the “C” (consolidative pattern), which coincides with the typical patterns seen in patients with COVID-19 described by Jackson et al (10).
It was not possible to demonstrate a statistically significant relationship of the LUSS greater than 18 points, in the evaluation of 12 spaces, with the death of the patients as the final outcome (p=0.9>0.05). A certain association that could be predictive was not demonstrated as opposed to the study by Ramos C et al (2) which refers that the 14 space LUSS has an excellent predictive capacity. However they report that it is inferior to already known laboratory markers such as CRP and LDH. The lack of statistically significant association in our study is probably due to the size of the sample. Despite not having demonstrated a statistically significant association between the final outcomes of patients with the lung ultrasound patterns or the LUSS, except for the aspects already mentioned as ultrasound findings of poor prognosis, our findings agree with the study by Tung-Chen Y et al (6) which states that lung ultrasound is an excellent tool for the characterization, monitoring and follow-up of patients with COVID-19. A study by Smith M et al (7) states that ultrasound provides us with the necessary information for the management of respiratory failure. Ultrasound also provides us with information on the basis of which the use of respirators could be prioritized in the epidemiological conditions of our environment, where the their availability is limited.
A statistically significant relationship was not demonstrated between death from COVID- 19 and a high LUSS value unlike the study carried out by Ramos C et al (2) in which they did show a relationship between the LUSS value and evolution of the patient, specifically with the need for mechanical ventilation. This supports the evidence from already known data that although we could not establish a relationship between LUSS and death as the final evolution of the patient, the aforementioned study reports that it can provide us with data to make timely decisions such as the use of mechanical ventilation.
The pulmonary alteration caused by COVID-19 in 11 or 12 lung regions evaluated by LUS, regardless of the ultrasound pathological pattern they present, as well as the presence of at least 6 regions with a subpleural consolidated pattern, have a statistically significant relationship with death in patients with a diagnosis of COVID-19, for which they can be considered as ultrasound indicators of poor prognosis, (p>0.01) and (p>0.05) respectively. No statistically significant relationship between death due to COVID-19 was found with the LUSS value itself, age older than 60 years, nor the presence of the pattern that could be more associated with death, that is, the alternate "B2" pattern with “C” (the value of p, in all the last mentioned ones, was less than 0.05).
REFERENCES:
World Health Organization. Weekly epidemiological update - 27 Octuber 2020.Available at: [who.int/publications/m/item/weekly-epidemio.. update---27-october-2020](who.int/publications/m/item/weekly-epidemio.. update---27-october-2020)
Ramos Hernández C, et al. Prediction of unfavorable evolution in patients hospitalized for COVID-19 using lung ultrasound. Arch Bronconeumol. 2020.DOI: 10.1016/j.arbres.2020.07.043. Available at: doi.org/10.1016/j.arbres.2020.07.043
Xing, C., Li, Q., Du, H. et al. Lung ultrasound findings in patients with COVID-19 pneumonia. Crit Care 24, 174 (2020). DOI: 10.1186/s13054-020-02876-9.Available at: doi.org/10.1186/s13054-020-02876-9.
Soldati Gino, MD et al. Proposal for International Standardization of the Use of Lung Ultrasound for Patients with COVID-19. J Ultrasound Med 2020; 39: 1413-1419. DOI: 10.1002/jum.15285. Available at: onlinelibrary.wiley.com/doi/full/10.1002/ju..
Gopar-Nieto R, Rivas-Lasarte M, Moya-Álvarez A, et al. Lung ultrasound for the identification of COVID-19 pneumonia. CardiovascMetabSci . 2020;31(Suppl: 3):178- 181. DOI: 10.35366 / 93944.
Tung-Chen Yale. Lung ultrasound in the monitoring of COVID-19 infection. Clinical Medicine 2020 Vol 20, Vol 20 No 4 July 2020. DOI: 10.7861 / clinmed.2020-0123 Available at: rcpjournals.org/content/clinmedicine/20/4/e62
Convissar D, Gibson L, Berra L. Application of Lung Ultrasound During the COVID- 19 Pandemic: A Narrative Review. Technology, Computing, and Simulation. August 2020 • Volume 131 • Number 2. DOI: 10.1213 / ANE.0000000000004929. Available at: pubmed.ncbi.nlm.nih.gov/32366774
Smith M. J, Hayward S. A, Innes S. M, Miller A.S.C. Point of care lung ultrasound in patients with COVID-19 a narrative review. Anesthesia 2020, 75, 1096–1104. DOI: 10.1111 / anae.15082. Available at: pubmed.ncbi.nlm.nih.gov/32275766
Bouhemad B, Dransart-Rayé O, Mojoli F, Mongodi S. Lung ultrasound for diagnosis and monitoring of ventilator - associated pneumonia. Ann Transl Med 2018; 6 (21): 418.DOI:10.21037/atm.2018.10.46Available at: atm.amegroups.com/article/view/22210/21649
Jackson K, Butler R, Aujayeb A. Lung ultrasound in the COVID-19 pandemic. Postgrad Med J 2020; 0: 1–6. DOI: 10.1136 / postgradmedj-2020-138137. Available at: [researchgate.net/publication/344161048_Lung.. -19_pandemic](researchgate.net/publication/344161048_Lung.. -19_pandemic)